Demography of Pediatric Primary Care in Europe: Delivery of Care and Training
Manuel Katz, MD*; Armido Rubino, MD‡; Jacqueline Collier, PhD§; Joel Rosen, BA; and Jochen H. H. Ehrich, MD¶
Abstract
Objective. The Union of National European Pediatric Societies and Associations recognized the lack of information regarding demography of delivery of care and training for the doctors who care for children in Europe. Therefore, the Union of National European Pediatric Societies and Associations studied factors and explanations for the variation between countries regarding pediatric primary care (PPC) and community pediatrics (CP) as well as the extent of formal training provided for those who take care of children at the community level.
Methods. An explanatory letter and a questionnaire with 12 questions regarding delivery of PPC and CP and training was mailed to the president of each of 41 national pediatric societies in Europe. Statistical data about population, country’s income, and infant mortality rate (IMR) were also obtained from World Health Organization data. Statistical analysis using multivariate and linear regression was conducted to ascertain which variables were associated with IMR. Descriptive statistics regarding demography and training are also reported.
Results. In 1999, a total of 167 444 pediatricians served a population of 158 million children who were younger than 15 years and living in the 34 reporting European countries. The median number of children per pediatrician was 2094; this varied from 401 to 15 150. A pediatric system for PPC existed in 12 countries; 6 countries had a general practitioner system, and a combined system was reported from 16 countries. Pediatricians did not work at the primary care level at all in 3 countries. In 14 of 34 countries, pediatricians worked in various aspects of community medicine, such as developmental pediatrics, well-infant care, school physicians, and so forth. IMR was lower in countries with a higher income per capita. In addition, a pediatric system of primary care had a protective effect when looking at IMR as the outcome. In 75% of the countries, some form of training in pediatric care for pediatricians was reported; the corresponding data for general practitioners was 60%. Community- based teaching programs were offered to pediatricians and general practitioners in a minority of countries only.
Conclusions. At the end of the century, Europe showed a considerable variation in both delivery of PPC and training for doctors who care for children. This study identified 3 different health care delivery systems for PPC, as well as 2 types of pediatricians who work in community-based settings. Formal training in PPC or CP for both pediatricians and general practitioners varied from established curricula to no teaching at all. Economic and sociopolitical issues, professional power, and geographical and historical factors may explain the differences in pediatric care among European countries.
Pediatrics 2002;109:788 –796; primary care, ambulatory pediatrics, delivery of care, training in primary care, European pediatrics.
Abbreviations. UNEPSA, Union of National European Pediatric Societies and Associations; PPC, pediatric primary care; CP, community pediatrics; IMR, infant mortality rate; CI, confidence interval; CME, continuous medical education.
From the *Department of Pediatrics, Soroka University Medical Center, Primary Care Unit, Ben Gurion University, Beer-Sheva, Israel; ‡Department of Pediatrics, University of Naples, Italy; §Division of Child Health, Faculty of Medicine, University of Nottingham, United Kingdom; MD Program in International Health and Medicine, Ben Gurion University, Beer-Sheva, Israel; and ¶University Children’s Hospital, Medical School, Hanover, Germany. Received for publication Jun 29, 2001; accepted Dec 11, 2001. Reprint requests to (M.K.) Department of Pediatrics, Soroka University Medical Center, Beer Sheva, Israel. E-mail: manuel@bgumail.bgu.ac.il PEDIATRICS (ISSN 0031 4005). Copyright © 2002 by the American Academy of Pediatrics.
Definitions:
1. We define a pediatrician as a physician who finished his formal training for pediatrics approved by the local health authorities or academic bodies in the country (either after undergraduate or as postgraduate education training).
2. A primary care pediatrician is defined as a type of pediatrician who offers curative and preventive services for acute and chronic problems in outpatient or ambulatory settings such as dispensaries, primary care clinics, health centers, or private practices.
3. Pediatricians and primary care pediatricians may work part-time or full-time.
4. We define the primary care system for children according to the proportion of the country’s children aged less than 15 years seen by either pediatricians or family physicians/general practitioners:
4.1. The pediatric system has more than 75% of children under the care of pediatricians.
4.2. The combined system has both pediatricians and general practitioners offering primary care to almost equal numbers of children ( 25%).
4.3. The general practitioner/family doctor system has more than 75% children seen by family physicians/general practitioners.
5. We define a community pediatrician as a pediatrician who devotes to the comprehensive recognition and understanding, prevention, and treatment of community-related health problems such as child protection, children in need, behavior problems, teenager approach, growth and developmental assessment, school medicine, etc.
The Union of National European Pediatric Societies and Associations (UNEPSA) held a symposium in 1997 in Warsaw, Poland, on pediatric primary care (PPC) and community pediatrics (CP). The presidents of 21 national pediatric societies in Europe reported on the structure of PPC and CP in their countries. Three different patterns of PPC were found in Europe: 1) pediatrician-led, 2) general practitioner–led, and 3) combined service. The reasons for the differences in service provision remained unclear. UNEPSA therefore developed a questionnaire on PPC and CP, which included questions about pediatric training and was sent to all European pediatric societies. This article contains data on geographical factors, age profile of the population, and socioeconomic factors that affected pediatric care in European countries in 1999.
Methods
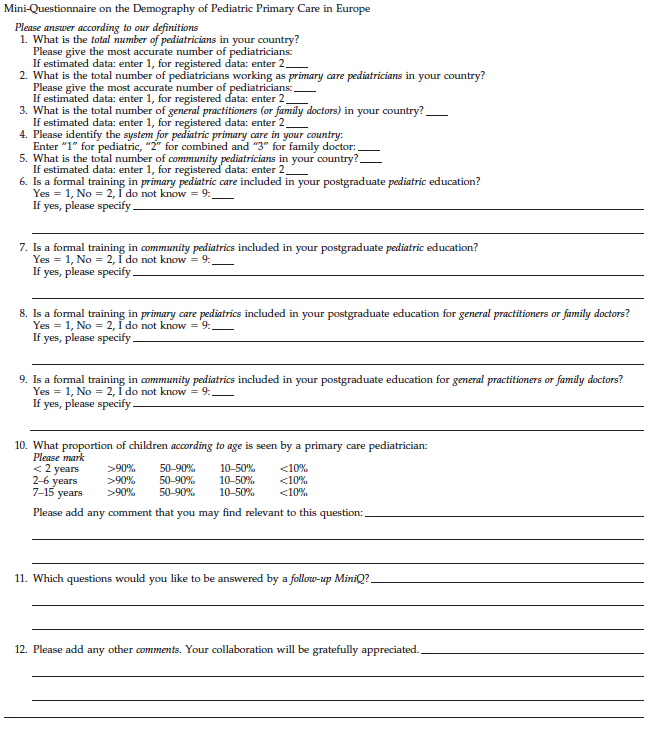
A questionnaire was mailed to the president of each of the 33 national pediatric societies that belong to UNEPSA and to 8 nonmember countries in Europe. UNEPSA includes the countries from the European Union, Scandinavia, and Eastern and Central Europe, as well as Turkey, Switzerland, and Israel. A letter explaining both the purpose of the project and definitions was included with the questionnaire. The questionnaire contained 10 specific questions regarding delivery of care and training of different types of doctors who work in PPC and CP. Also, 2 open questions for comments were included (Table 1). In calculating the number of pediatricians and primary care pediatricians, both parttime and full-time pediatricians were included.
The following information was obtained from the World Health Organization: overall population, population younger than 15 years, infant mortality rate (IMR), and income per capita. IMR was used as a crude indicator of a nation’s child health status. Analysis of variance was used to explore the association between the type of primary care system and the country’s income per capita. Linear regression was conducted to ascertain which factors were associated with IMR. With IMR as the outcome, the system of PPC, income per capita, and the proportion of the population younger than 15 years were entered as explanatory variables. System of care was entered using dummy variables, income per capita was entered as per 1000 US dollars, and backward selection was the entry method used. The final model had an adjusted R2 value of 0.46 with income and pediatric system of care as the predictors (P .001, 0.711, 95% confidence interval [CI]: 0.983 to 0.438; P .034, 5.416, 95% CI: 10.383 to 0.450, respectively). Descriptive statistics regarding demography and training were used.
Results
Responses were received from 34 countries (83% response rate); no data were available from Albania, Belarus, Bosnia, Malta, Moldavia, Rumania, or Yugoslavia. Results reported are for these 34 countries unless otherwise specified.
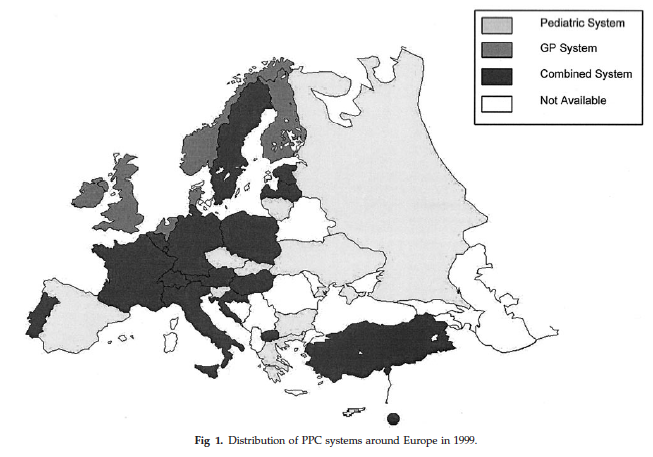
Delivery of Care
The total number of pediatricians reported at the end of 1999 was 167 444, serving a population of approximately 158 million children who were younger than 15 years. The median number of children per pediatrician was 2094. This number varied widely between countries, ranging from 401 to 15 150. Twelve of the 34 countries had a pediatric system for primary care for children, 6 had a general practitioner/family doctor system, and 16 had a combined system for the care of children who are younger 15 (Fig 1). Three Eastern European countries (Bulgaria, Croatia, and Czech Republic) reported public health reform in progress, including a shifting from the pediatric system to the combined system. Three countries (8%) did not have any pediatricians working at the primary level of care. Fourteen countries (41%) reported having community pediatricians.
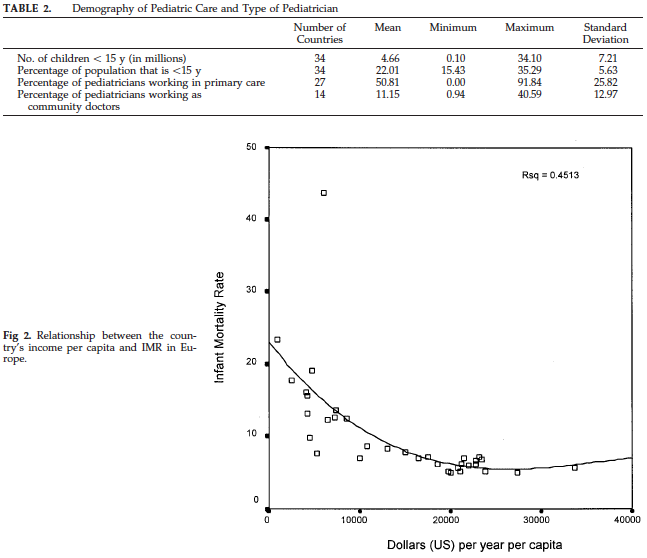
The child populations in the European countries varied considerably, ranging from 0.1 to 34 million (Table 2). The proportion of children with respect to the total population also varied from 15% to 35%. The type of pediatricians showed a wide variation: the proportion of pediatricians considered to deliver primary care ranged from 0% to 92% or in community care from 1% to 41%.
IMR showed an inverse relationship to national income (r 0.67), indicating that 45% of a country’s IMR could be predicted from the country’s wealth (Fig 2). The type of pediatric primary care system was significantly associated with the income of the country (F 6.35, df 2, P .005; Fig 3). A post hoc test revealed that those countries with a pediatric system had significantly lower incomes per capita than those countries with either the general practitioner system (mean difference: $13 154; 95% CI: $5350–$20 957; P .002) or the combined system (mean difference: $7288; 95% CI: $1197–$13 380; P .02).
Higher income per capita and a PPC system were protective factors and were associated with a reduction in the IMR. This statistical model used suggests that every $1000 increase in per capita income is associated with a decrease of 0.711/1000 in the IMR ($10 000 associated with a decrease of 7.11/1000 and so forth) and, when income is held constant, the PPC system compared with the other systems is associated with a decrease of 5.4/1000 in IMR.
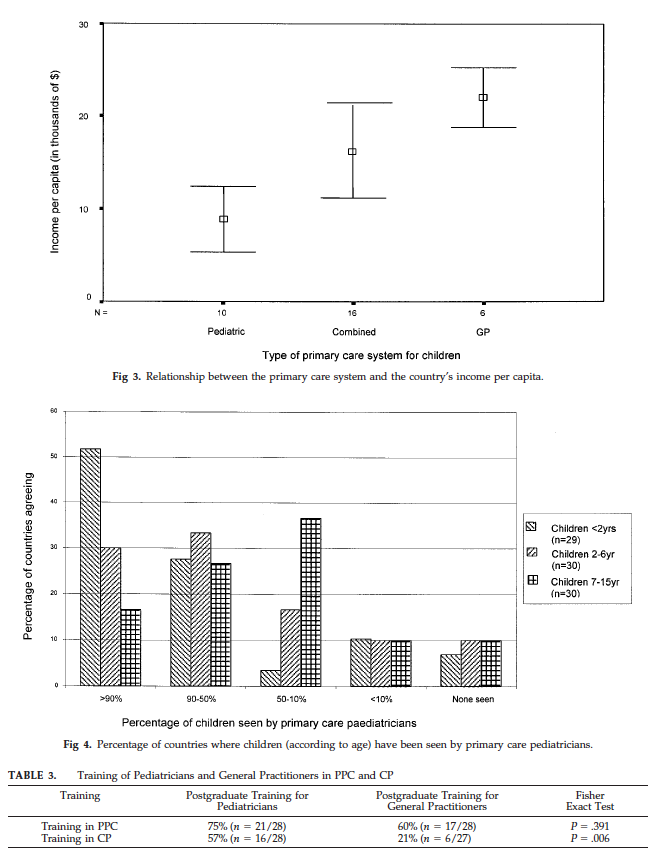
The proportion of countries that have children who are seen by pediatricians at the primary care level varied across the 3 age groups defined in the questionnaire (Fig 4). In 52% of the countries, 90% of the children who were younger than 2 years were seen by primary care pediatricians; this proportion was considerably less in children who were 7 to 15 years of age: pediatricians saw 90% of the older children only in 18% of the countries. Almost 10% of the countries reported that pediatricians were not involved at all in the care for children at the first level of care at any age.
Organization of Training
Data from the questionnaires regarding postgraduate training for PPC and CP was available for 28 of 34 countries. Postgraduate education in primary care was offered to pediatricians in 75% of countries and to general practitioners in 60%. Training in CP was more frequently offered to pediatricians than to general practitioners (Table 3).
Thirty countries provided additional information regarding the nature and content of the training programs for pediatricians (Figs 5 and 6). Three different types of training were reported: training in primary care and CP as part of the national pediatric training program (mainly hospital-based), a communitybased program, and continuous medical education program (courses, workshops). Five countries reported a lack of formal teaching in primary care, and 7 did not have any training in CP.
Discussion
During the past 23 years, since the Alma-Ata declaration, 1 primary health care in general and PPC specifically have been shown to be important for the care of the sick child and in improving the general health of the population. “Health care for all by the year 2000” is a cliche that has long been discarded as a euphoric dream. Even in the European countries there are major differences in level, quality, and type of care given to the pediatric population. The UNEPSA understood that; although the World Health Organization’s famous statement has not yet been achieved, the need to move closer to such a goal could only take place once the current status of care is known. In an attempt to elucidate the demographics of pediatric primary care in Europe, we begin this discussion with a description of the current situation followed by an analysis of what is best in addressing children’s health needs.
When the last century came to a close, 167 444 pediatricians were attending to a pediatric population of 159 million patients who were younger than 15 years and living in the 34 reporting European countries. Three different systems of PPC existed in Europe. Of the 3, 12 of the 34 countries had a pediatric system of primary care, 6 had a general practitioner/ family doctor system, and the majority, 16, had both systems coexisting. It is interesting that 3 of the countries, all from Eastern Europe, reported to be shifting from a pediatric system to a combined system. In addition, 3 countries did not have any pediatricians working at the primary care level. As expected, these are the countries that had a general practitioner system in place. Fourteen countries had community pediatricians, which may show that preventive measures were considered a priority in fewer than half of the 34 countries surveyed.

The distribution of the 3 systems throughout Europe illustrates the long-standing argument in academic literature2–5 as to who is the preferred doctor treating children in the community. Those countries that use general practitioners and family physicians in a primary care setting show a clear disadvantage when taking into account CP. Most general practitioners have a lack of training in dealing with CP concerns such as mental health, immunizations, and other preventive measures. Traditionally, family and general practitioners deal more with the acutely ill child, and other health professionals are responsible for community care.
The Court committee6 in its report in 1976 described a dichotomy in pediatric care in England. The committee recognized that the issues that affected children in the last quarter of the 20th century in England were no longer acute and episodic illness but rather issues that should be dealt with by trained community pediatricians. Morbidity in the pediatric community as a result of chronic illness, disabilities, psychiatric disorders, and ill health arising from family stress are concerns that general practitioners who work under the national health system do not have the time or the training to deal with. During the past 2 decades, an improvement has taken place in the United Kingdom. With a pediatric population growth of only 1.5 million children, the number of community pediatricians has approximately quadrupled from 86 to 364.7 This laudable trend, however, is achievable only in a limited number of countries that are relatively rich and have the resources for a dual system of child care.8 However, countries with the pediatric system offered particular advantages, especially those with a low gross national product. Analyzing infant mortality, the PPC system was associated with reduced IMR compared with other systems. Most of those pediatric systems (excluding Spain, Greece, and Cyprus) were part of the former communist countries. The most significant problem is the great delay in advancement of medical technology and standard of treatment in these countries compared with their Western counterparts.9 This has been improving significantly now that the government no longer discourages international collaboration as it did before 1993.
The most extensive system, also showing the greatest variation, is the combined system. Basically, the variation depends on the amount of children treated by general practitioners or pediatricians. Half of the reporting countries that were using the combined system had 90% of the pediatric population that was younger than 2 years being treated by pediatricians only and a variable percentage of pediatricians who treat the older children. It is strongly believed that every country needs pediatricians who have the training in treating and preventing sickness in the most vulnerable phase of childhood. The variation in the type of doctor who cares for children on a community level can be explained partially by geographical factors: in some countries, such as Switzerland, pediatricians are the only primary caregivers in the cities. In the more rural areas, where the population is more dispersed, there is a shift to family physicians treating the entire population, including young children. The question that immediately arises is, who, then, is in charge of the preventive measures needed in such a community? In the Italian model,10 pediatricians do work under the national health services system and care for 85% of children who are younger than 6 years. Preventive measures, such as immunizations, are the responsibility of a different national health services community service of the mother and child health departments.
Three of the 34 countries plan to change from an exclusively pediatric system to a combined system. There is no obvious reason for this change except that all of these countries are undergoing a major health care reform. In Bulgaria, the Health Insurance Act of 1998 is probably the reason for the change. During the decade of the transitional process into a capitalistic economy, the public health care services in Bulgaria were deteriorating. The lack of health care finance was a major reason for the poor performance of the Bulgarian public health care sector. Bulgarian policy makers decided that an insurancebased financial mechanism could help to rescue the failing public health care services.11 Croatia is undergoing a similar change, which may threaten the preventive care readily available in the former socialist system.12 It remains to be shown that these changes will be beneficial with regard to preventive measures, especially for children. The question is whether the change from a public health care system to a private one also includes a necessary change of medical specialties in a given country. The initial response is that in the short term, all practicing doctors would do their best to adjust to the new system. Bulgaria, for example, has declared that it will shift drastically from a pediatric system to a general practitioner system. Patients will then be referred to pediatricians from general practitioners, and fewer pediatricians will be needed because they will work as specialists only. It is unclear what will happen to those pediatricians who are no longer needed. It could be imagined that in the long run they will have to be trained as family doctors.
Six of the reporting countries indicated that the reason for having the combined system is the variable population density within the country, which means that children who live in the more highly populated areas were treated by pediatricians and out in the more rural areas children were lumped together with the rest of the population and cared for by family physicians. This means that these countries have a mixture of both a pediatric and a general practitioner system in parallel, instead of a truly combined system. For financial reasons, it is clearly inadequate to keep specialized doctors in rural areas. 13 The question is, do patients in rural parts of Europe get equal standards of care as their counterparts in the urban regions? Moscovice and Rosenblatt14 discussed this issue as it applies to the United States under a managed care system. This question, applied to Europe, remains open. However, if we consider the American model, a very important issue is the special training of family physicians to work in rural communities.15 Our data show that there is a very large discrepancy between the amount of training given to European family physicians and to pediatricians in both primary and community care. The care for pediatric patients in rural settings is also very much influenced by the economic burden, work load, and relatively lower income of the physician working in villages or on islands. Recruiting physicians in general and specialists in particular to work in remote areas is difficult.16
Our data on demography of training in European countries in both PPC and CP show that postgraduate training in PPC was offered to pediatric residents in 75% of the countries but to family medicine residents in only 60%. Countries that have a pediatric system did not necessarily have a primary care training program. Furthermore, some countries with a general practitioner system offered primary care pediatrics as part of the pediatric residency training, although most of these doctors would not end up working in such a setting but will be part of the specialist referral system. These paradox situations are rather perplexing, and in an attempt to explain such occurrence, we come up shorthanded.
In the turmoil of the discussions on the planned health reforms in Europe, it became clear that the decision-making processes for a better economic and/or medical rationale are often not in the hands of the health care professionals. Training recommendations, however, are most often institutionalized following the advice of the medical schools and health organizations in the country.
The residents’ attitude and practice can be molded in the early stages of their pre- and postgraduate work.17–19 Furthermore, pediatric residents who have an interest in working in the primary setting find it helpful to spend part of their training out in the community in private office settings.20 Once in the workforce, the importance of continuous medical education (CME) is beyond measure because, at times, doctors are caught up in their daily work and are not able to keep up with the advances in medical care. CME programs must be implemented to maintain high standards of care outside the academic environment in the community.21 We have found that only 9 countries had CME programs in PPC.
It is also somewhat alarming when discussion turns to CP. Only 57% and 21% of reporting countries offered training in CP for pediatric and general practitioner residents, respectively. This becomes a concern at times when morbidity in pediatrics is not dominated by acute illnesses but more often by chronic or psychosocial problems, which without upto- date training can be missed.22 We agree with the American Academy of Pediatrics in its statement on the “pediatrician’s role in community pediatrics,”23 but it should not stop here. Countries that have the children’s best interest in mind need to include more training sessions in programs for both pediatricians and family doctors. Crouchman et al24 suggested, following the Bordeaux meeting, that social community pediatrics become a subspecialty. The focus should be on training, which must start at the undergraduate level.
Our critics may ask why use IMR as the indicator for child health. IMR is an excellent indicator in the developing world where figures of IMR are high and a change is significant enough to be used as a gauge for the effectiveness of program interventions. In Europe, especially in Western Europe, where IMR varies below 8/1000, the indicators for the pediatric status of health have to include older children. Such indicators are vital to compare between countries for the purpose of developing and promoting interventions and reform in the delivery of care for all children. Unlike the past, when children died in infancy because of malnutrition and disease, today pediatric mortality and morbidity are affected by more complex causes.25 Adolescent suicide has become the third major cause of death in that age group.26 Accidents and child abuse, too, are major components of child mortality and morbidity. The problem is that we do not currently have any better measures for improving the current health status, but we challenge the academic and professional communities to consider this as we enter the new century and attempt to improve still the health status of our children.
Conclusion
The care of children at the primary care level in Europe, at the beginning of the new century, varied between and within countries. Economic, geographical, and historical factors contribute to the intrinsic and extrinsic variations, as well as the role of different types of pediatric care. Training in PPC and CP varied from a well-established program to a total lack of teaching. IMR and income per capita were valuable indicators for the status of health in Europe. However, it seems to be necessary to look for new measures regarding sociopsychocultural differences and changes when comparing the health status of the pediatric population in the richer countries. There are national differences in pediatric care across Europe and these idiosyncrasies require additional study. This would enable countries to learn more from one another and to identify the factors that have an impact on the type of primary health care system provided for children and to avoid making major policy decisions while not taking into account the most important factors, such as the child’s well-being.
Acknowledgments
We are indebted to the representatives of the European national pediatrics societies and associations: Andersen (Denmark); Angeloni (Italy); Babel (Switzerland); Baranov (Russia); Basaran (Turkey); Basys (Lithuania); Bauche (Belgium); Baum/Blair (United Kingdom); Benedick Dolni/Hribar (Slovenia); Bikis (Latvia); Constadopolus (Greece); Conter (Luxembourg); Cordeiro (Portugal); Delgado Rubio (Spain); Dluholucky (Slovakia); Grunberg/Riikjarv (Estonia); Hallman (Finland); Holl (Netherlands); Horkelsson (Iceland); Janda (Czech Republic); Kalaikov (Bulgaria); Katz (Israel); Kawalek (Poland); Kocova (Macedonia); Kriz (Croatia); Larson (Sweden); Lukyanova (Ukraine); Lunde (Norway); Mc Kiernan (Ireland); Olah (Hungary); Pelz (Germany); Persianis (Cyprus); Schmitz (France); and Zaunschirm (Austria).
References
1. Declaration of Alma-Ata. Lancet. 1978;2:1040–1041
2. Marsh GN, Russell D, Russell IT. Is pediatrics safe in general practitioners’ hands? A study in the north of England. J R Coll Gen Pract. 1989;39:138–141
3. Westbom L. Pediatricians in primary health care—do general practitioners and pediatricians talk the same language? Lakartidningen. 1992;89: 2300–2301
4. Gerard JM, Klasner AE, Madhok M, Scalzo AJ, Barry RC, Laffey SP. Poison prevention counseling: a comparison between family practitioners and pediatricians. Arch Pediatr Adolesc Med. 2000;154:65–70
5. Leduc DG, Pless IB. Pediatricians and general practitioners: a comparison of the management of children with febrile illness. Pediatrics. 1982; 70:511–515
6. Court D. (Chairman). Fit for the Future, the Report of the Committee on Child Health Services. London, England: H. M. Stationery Office, Cmnd. 6684; 1976
7. Paediatric Services Within the Community for the New Millennium. Report of a Working Party: Royal College of Paediatrics and Child Health. London, England: Royal College of Paediatrics and Child Health; 1999
8. Bhrolchain CN. Will deprived areas still need community paediatricians? An unpopular hypothesis. Public Health. 1994;108:319–323
9. Janda J. Paediatric care in the Czech Republic. Arch Dis Child. 1995;72: 271–273
10. del Torso S, Bussi R, DeWitt TG. Primary care pediatrics in Italy: eighteen years of clinical care, research, and teaching under a national health service system. Pediatrics. 1997;99(1). Available at: http:// www.pediatrics.org/cgi/content/full/99/1/e8
11. Pavlova M, Groot W, van Merode F. Appraising the financial reform in Bulgarian public health care sector: the Health Insurance Act of 1998. Health Policy. 2000;53:185–199
12. Chen MS. Health care reform in Croatia: for better or for worse? Am J Public Health. 1988;88:1156–1160
13. Crane M. Is doctors’ hard work paying off? Med Econ. 1993;70:100–108, 111–112
14. Moscovice I, Rosenblatt R. Quality-of-care challenges for rural health. J Rural Health. 2000;16:168–176
15. Talley RC. Graduate medical education and rural health care. Acad Med. 1990;65(suppl):S22–S25
16. Broffman G. How can pediatric care be provided in underserved areas? A view of rural pediatric care. Pediatrics. 1995;96:816–821
17. Lesky LG, Hershman WY. Practical approaches to a major educational challenge. Training students in the ambulatory setting. Arch Intern Med. 1995;155:897–904
18. Margolis CZ, Barak N, Porter B, Singer K. The community-oriented primary care clerkship. Isr J Med Sci. 1987;23:1027–1034
19. Porter B. A community internship as a continuation of a communityoriented curriculum. Acad Med. 1990;65:780–781
20. Ponitz KL, Needlman RD, Kilkenny TJ. Primary care relationships in pediatric hospital clinics vs private offices. Arch Pediatr Adolesc Med. 2000;154:1209–1213
21. Martinez Ros MT, Ballesteros Perez AM, Molina Duran F, Sanchez Sanchez F, Soto Calpe R. Continuing education in primary care: needs perceived by physicians, pediatricians, and nursing staff. Aten Primaria 1996;17:124–126
22. Frankenfield DL, Keyl PM, Gielen A, Wissow LS, Werthamer L, Baker SP. Adolescent patients: healthy or hurting? Missed opportunities to screen for suicide risk in the primary care setting. Arch Pediatr Adolesc Med. 2000;154:162–168
23. American Academy of Pediatrics, Committee on Community Health Services. The pediatrician’s role in community pediatrics. Pediatrics. 1999;103:1304–1307
24. Crouchman M, Pechevis M, Sandler B. Social paediatrics and child public health—a European perspective. Arch Dis Child. 2001;84:299 – 301
25. Melinder KA, Andersson R. Stable and dynamic differences in injury mortality between the Nordic countries. What do they say about inherent national characteristics with regard to risk? Scand J Public Health. 2000;28:16–22
26. Madge N. Youth suicide in an international context. Eur Child Adolesc Psychiatry. 1999;8:283–291
FIVE ‘‘W’ QUESTIONS
“Good descriptive research, like good newspaper reporting, should answer five basic ‘W’ questions—who, what, why, when, and where—and an implicit sixth question, so what?
Who had the disease in question?
Why did the condition or disease arise?
When is the condition common or rare?
Where does or does not the disease or condition arise?
So what? The implicit ‘W’ relates to the public health effect.“
Grimes D, Schulz KF. Descriptive studies: what they can and cannot do [review]. Lancet. 2002;359:145–149
Submitted by Student
Click here to download the presentation



